Pelvic Floor Disorders
What are Pelvic Floor Disorders (PFD)?
Pelvic floor disorders include pelvic organ prolapse, urinary incontinence, anal incontinence and pelvic pain.
When do they occur?
These disorders can occur at any time in adulthood however they are most common during the perimenopausal and post-menopausal years.
Can you have more than one disorder?
Yes.
What is pelvic organ prolapse (POP)?
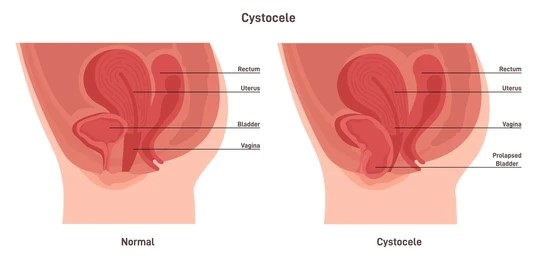
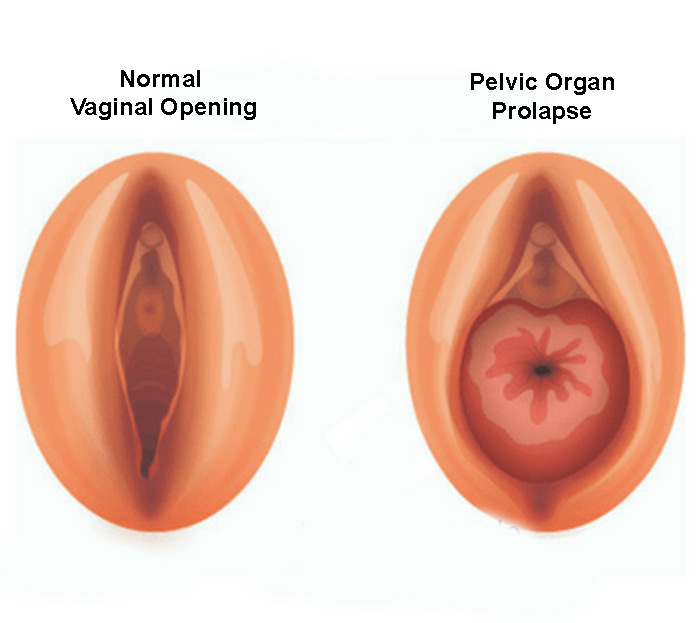
Prolapse refers to a descent or drop in the bladder, the uterus or the rectum to or through the vaginal opening. It is possible to have descent of all three organs simultaneously.
- Cystocele – dropped bladder
- Rectocele – dropped rectum
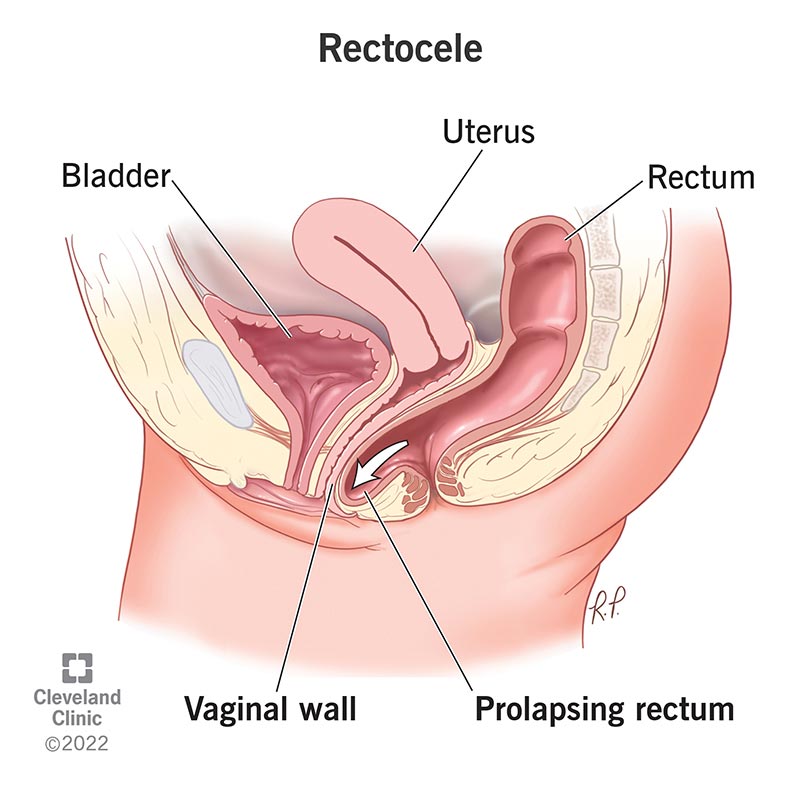
Reference: https://my.clevelandclinic.org/health/diseases/17415-rectocele
** This is different from a prolapsing rectum. - Uterine prolapse – dropped uterus
Reference: https://femalehealthawareness.org/en/pelvic-organ-prolapse/
What causes pelvic organ prolapse?
Weakness of or injury to pelvic floor muscles, support structures or nerves leads to pelvic floor disorders.
What are some contributing factors or causes of PFD?
- Pregnancy and multiple vaginal deliveries.
- Injury to pelvic muscles or anal sphincter.
- Large babies delivered vaginally.
- Operative deliveries.
- Connective Tissue Diseases like Ehler Danlos.
- Conditions like diabetes, menopause.
- Genetics.
- Activities: persistent and prolonged heavy lifting, coughing etc.
How is pelvic organ prolapse assessed?
The degree of prolapse is determined based on the degree of descent i.e. how far above or below the hymen the prolapsing organ is.
There are 4 grades:
- Grade 1 & 2 – the prolapse remains within the vaginal canal above or up to the level of the hymen.
- Grade 3 & 4 – the prolapsed organ protrudes through the vaginal canal and past the hymen.
How do you treat pelvic prolapse?
There are 3 management options:
- Expectant management - no active treatment or intervention, usually because it is not symptomatic or the prolapse does not cause the woman any harm or discomfort.
- Pessary – small silicone devices that are inserted into the vagina to support the prolapsing organ. This device is easy to maintain at home and allows the woman to forgo surgery. May cause mild vaginal discomfort, vaginal spotting or increased vaginal discharge.
Pessaries

Reference: Lamers BH, Broekman BM, Milani AL - International urogynecology journal (2011).
- Surgery:
There are various options available including:- Hysterectomy.
- Ligament suspensions.
- Anterior repair.
- Posterior repair.
- The type of prolapse.
- The severity of the prolapse.
- The presence or absence of urinary or anal incontinence.
- The patient`s desire for penetrative sexual intercourse.
- The patient`s medical conditions etc.
What is anal incontinence (AI)?
Anal incontinence refers to loss of gas, stool or mucus through the anus.
What is fecal incontinence (FI)?
Refers to loss of stool, liquid or solid, or mucus through the rectum. It is common practice to use the terms fecal and anal incontinence interchangeably.
What causes anal or fecal incontinence?
- Constipation.
- Medication.
- Neurological issues.
- Injury to the anal sphincter complex.
- Functional or physical immobility.
- Age.

How do you manage or treat AI?
- Dietary modifications.
- Stool softeners, stool bulking agents etc.
- Exercise and weight loss.
- Wearing anal incontinence products like anal pads, anal plugs and or inserts.
- Repair or replacement of the anal sphincter complex.
- Nerve stimulation.
- Creating an alternative outlet – ostomy.
What is urinary incontinence (UI)?
It is the involuntary loss of urine.
What are the different types of UI?
- Stress UI.
- Urge UI/Overactive Bladder
- Mixed UI.
- Coital incontinence.
- Orgasm associated incontinence.
- Overflow incontinence.
- Many others.
What is Stress Urinary Incontinence?
Leakage of urine during activities that are associated with increased abdominal pressure like coughing, sneezing, standing up from a seated position etc.
What causes SUI?
Caused by increased external pressure on the bladder that surpasses that of the urethral sphincter complex.
What is Urge Incontinence (UUI)?
Loss of urine associated with sudden, uncontrollable urge to empty one`s bladder.
What causes UUI?
Caused by sudden uncontrolled bladder spasms that present as the sudden urge to urinate.
What is coital incontinence?
Loss of urine that occurs during penetrative sex.
What is orgasm related incontinence?
Leaking urine at the time of orgasm.
How do you treat urinary incontinence?
Treatment of UI will depend on the type of incontinence that a patient has.
Treatment options include:
- Behavior modification and bladder training exercises.
- Sub urethral slings.
- Medication.
- Pelvic floor physical therapy.
- Botox injections.
- Urethral bulking.
- Pessaries.
Menopause and Pelvic Floor Disorders

Pelvic floor disorders usually become apparent or symptomatic in the perimenopausal and post-menopausal years.
In many women, menopause becomes the inciting factor for pelvic floor disorders, given the central role that estrogen and progesterone play in this phase of life.
The use of hormonal therapy is a key part of managing symptoms caused by menopause and PFD, and vaginal estrogen is the preferred form of treatment alongside other treatment modalities.
Use of hormonal therapy is not without risks and the discussion and decision to employ hormone therapy as part of the treatment regimen is a key part of the patient clinician interaction.