Hysterectomy: Frequently asked questions
Hysterectomy is one of the most common gynecologic surgeries performed today. The procedure is performed for many reasons including: abnormal uterine bleeding, fibroids, endometriosis, chronic pelvic pain, uterine prolapse and cancers – uterine, ovarian, cervical, etc.
What is it?
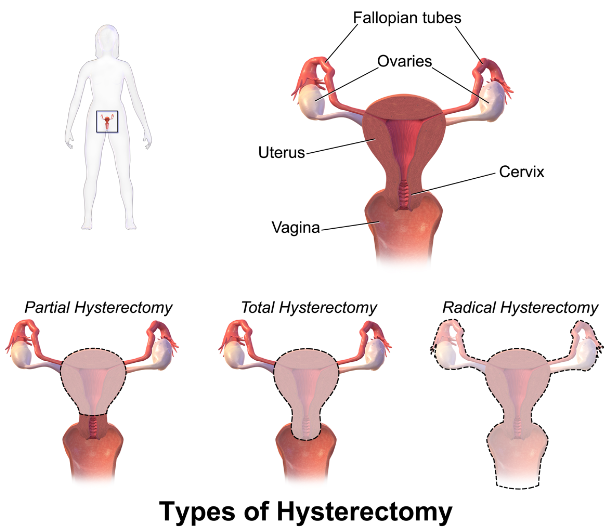
A surgical procedure that removes the uterus (womb). Your doctor may also take out the cervix at the same time (total hysterectomy). If only the uterus is removed, then it is referred to as a partial or subtotal hysterectomy. Radical hysterectomy - the uterus and neighboring organs are removed.

What other organs can be removed at time of hysterectomy?
Fallopian tubes and or ovaries. If both fallopian tubes are removed, the procedure is referred to as bilateral salpingectomy. If both ovaries are removed, it is referred to as bilateral oophorectomy.
After a hysterectomy will I need to continue getting pap smears?
If the cervix is not removed, you will need to continue with cervical cancer screening. If the cervix is removed and you do not have a history of abnormal pap smears then you will not require subsequent pap smears. Women with a history of abnormal pap smears or with history of immunosuppression who have had a total hysterectomy will need to discuss future pap testing with their doctor.
What are the different routes of hysterectomy?
Route refers to how the surgeon performs the surgery.
- Vaginal hysterectomy – the uterus is accessed and removed through the vagina. The surgery is performed through the vagina and there are no incisions on the abdomen.
- Abdominal Hysterectomy – the uterus is accessed and removed through an incision on your abdomen.
- Laparoscopic Hysterectomy –In this procedure, the surgeon operates through 3-5 small incisions on your abdomen.
- Laparoscopic assisted vaginal hysterectomy – is a procedure that combines both laparoscopic and vaginal routes ie part of the surgery is performed laparoscopically and the other part is performed through the vagina.
- Robotic assisted hysterectomy – The surgeon uses a robot and works through multiple small incisions on your abdomen. Both the laparoscopic and the robotic assisted hysterectomies are considered minimally invasive procedures.
What determines the route of hysterectomy?
This decision will be made by you and your doctor. Some of the factors that go into decision making include, the reason for the surgery eg bleeding, fibroids, cancer, prolapse- other procedures that need to be performed at the time of surgery, previous surgeries, other medical conditions like obesity, COPD etc Availability of resources and physician experience are also a consideration.
How long will I be in the hospital?
our hospital stay depends on the route of hysterectomy, extent of surgery and how you do post operatively. With minimally invasive hysterectomies – laparoscopic, laparoscopic assisted and robotic hysterectomies – and vaginal hysterectomies, patients may be able to go home the same day or the day after surgery. Abdominal hysterectomies may require 1-3 nights in the hospital.
What should I expect?
Before Surgery: Your last meal will be before midnight on the day of surgery. On the morning of surgery, you may have lab work performed if not done previously. If you are premenopausal the nurse may do a pregnancy test to confirm that you are not pregnancy. You will meet with your surgeon and the anesthesia team prior to being taken to the operating room.
After surgery you will likely be drowsy and feel tired. You may also experience some nausea and vomiting. Your surgical team will work to ensure that you are comfortable and that your pain is well controlled. You may have a urinary catheter – tube that drains your bladder – and compression socks or devices - on your legs that decrease your risk of blood clots. These will be removed once you are awake and able to walk around unassisted.
At time of discharge from the hospital, your team will discuss with you what activities you can engage in, what medications you can take for pain as well as what signs or symptoms you need to watch for and when to call the doctor when you are at home. You should not place anything in the vagina during your recovery period. Your doctor will inform you when to can resume sexual intercourse. You will also be required to schedule an outpatient follow up visit after surgery. Average recovery time from a hysterectomy is approximately 6 -8wks. Your doctor will inform you of when you can return to work as well as resume regular activity.
Lastly, your surgeon will advise you on any other additional issues specific to you.
What are the risks associated with hysterectomy?
Hysterectomy is generally a safe procedure, but as with all surgeries there is a risk of bleeding, infection, injury to neighboring organs and urinary retention. If your blood loss is large or you develop symptoms from the blood loss, you may need a blood transfusion. There is a small chance of getting an infection from the blood products. You may also need additional surgery if there are complications post-operatively.
Risks associated with receiving anesthesia are small but include risk of blood clots, stroke, heart attack and death. You will meet with your anesthesia team prior to surgery.